Hi Dr. Stein,
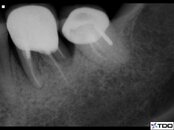
I had an exploratory surgery on tooth #3 at a local periodontist last Thu. Then plan was if the periodontist found the root is cracked, he would extract the tooth. However, there is no crack. He told me there was significant bone loss around the MB root, so he did a bone regeneration with some bone graft material. But he could not explain why I had the fistula on the gum.
However, I feel the situation is not getting better. I feel tooth #3 "sticks" out, meaning it feels longer than other teeth so when i clinch my teeth, the teeth at the right side (or tooth #3) touch the bottom teeth first. Also when I clinch tooth #3, i feel some slight pain at the root end.
I do not know what to do.. I will see the periodontist to remove the stitches next week. Maybe it is root end infection and apicoectomy is needed? Basically how can you judge if a root tip and its surrounding tissue are infected? Would you have to open the gum?
Thank you!
I had an exploratory surgery on tooth #3 at a local periodontist last Thu. Then plan was if the periodontist found the root is cracked, he would extract the tooth. However, there is no crack. He told me there was significant bone loss around the MB root, so he did a bone regeneration with some bone graft material. But he could not explain why I had the fistula on the gum.
However, I feel the situation is not getting better. I feel tooth #3 "sticks" out, meaning it feels longer than other teeth so when i clinch my teeth, the teeth at the right side (or tooth #3) touch the bottom teeth first. Also when I clinch tooth #3, i feel some slight pain at the root end.
I do not know what to do.. I will see the periodontist to remove the stitches next week. Maybe it is root end infection and apicoectomy is needed? Basically how can you judge if a root tip and its surrounding tissue are infected? Would you have to open the gum?
Thank you!