Laurence Stein DDS
Medical Moderator
Hi sbbi,
I went back to the original post in 2004 to bring myself up to speed. My responses that seemed so lucid at the time are even confusing me. Part of the problem is that the actual procedure the patient underwent was unclear.
At times references were made to root amputations, hemisections and retrograde fillings. They are all different procedures. It is also equally difficult to quickly describe each procedure... especially so a lay person can understand it.
You may be confused for the same reason that I find the old post confusing. In your question to me, I think your reference to a hole is referring to the socket hole left behind after a root is removed. On the other hand, the hole I am referring to is the one left behind when the tooth was sectioned and the pulp chamber was opened up as a result.... this is a hole in the tooth.
The socket "hole" will fill in by normal healing. Any hole or other perforation into the pulp chamber must be closed by the dentist. He will usually be doing the post and core followed by a cap or a permanent filling into the pulp chamber.
For a retrograde filling, the holes would be the ones created into the skin and bone to access the root end of the tooth and the hole created by the filling preparation in the end of the root. The hole through the skin and bone will close during normal healing and the hole in the root end must be filled with the retrograde filling.
Let me try to describe, more clearly, the different procedures listed in the original post. Perhaps it will make things easier to understand.
Soooo.... let's try again.
A HEMISECTION is a procedure in which a tooth with multiple roots are made separate by making a cut through the existing crown and all the way through to the supporting bone. The separate tooth sections are treated as if each is a separate tooth or if one of the separated tooth sections cannot be saved, then only that section is extracted and the remaining section is restored. Hemisection WITHOUT the removal of a separated section is often done to improve the restorative prognosis of a tooth with gum disease between the roots or in the event there is a fracture between the roots of a multi-rooted tooth.
The hemisection and subsequent removal of a root from a multi-rooted tooth is called a ROOT AMPUTATION. The hemisection cut may be vertical, horizontal or diagonal. It is often used as a "bail out" procedure to salvage an existing crown or bridge
Since the cut to separate the tooth passes through the nerve chamber in the middle of the tooth, a root canal procedure must be performed prior to the split. If there is an existing root canal in the hemisected tooth, then all that is needed to seal the opening that communicates with the nerve chamber. This can done using a cap or a filling. The technique used will vary from case to case.
A RETROGRADE filling is a filling that is placed into the root end (apex) of a tooth. It is typically used when a traditional root canal procedure cannot be used or when a traditional root can procedure is not successful and the tooth cannot be treated in a convention manner again.
Hopefully, I've managed to answer your question as confusing as all this seems to be.
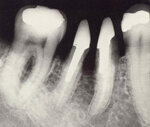
The photos left to right:
Retrograde filling, hemisected molar, hemisected molar under a bridge with one root amputated.
Regards,
I went back to the original post in 2004 to bring myself up to speed. My responses that seemed so lucid at the time are even confusing me. Part of the problem is that the actual procedure the patient underwent was unclear.
At times references were made to root amputations, hemisections and retrograde fillings. They are all different procedures. It is also equally difficult to quickly describe each procedure... especially so a lay person can understand it.
You may be confused for the same reason that I find the old post confusing. In your question to me, I think your reference to a hole is referring to the socket hole left behind after a root is removed. On the other hand, the hole I am referring to is the one left behind when the tooth was sectioned and the pulp chamber was opened up as a result.... this is a hole in the tooth.
The socket "hole" will fill in by normal healing. Any hole or other perforation into the pulp chamber must be closed by the dentist. He will usually be doing the post and core followed by a cap or a permanent filling into the pulp chamber.
For a retrograde filling, the holes would be the ones created into the skin and bone to access the root end of the tooth and the hole created by the filling preparation in the end of the root. The hole through the skin and bone will close during normal healing and the hole in the root end must be filled with the retrograde filling.
Let me try to describe, more clearly, the different procedures listed in the original post. Perhaps it will make things easier to understand.
Soooo.... let's try again.
A HEMISECTION is a procedure in which a tooth with multiple roots are made separate by making a cut through the existing crown and all the way through to the supporting bone. The separate tooth sections are treated as if each is a separate tooth or if one of the separated tooth sections cannot be saved, then only that section is extracted and the remaining section is restored. Hemisection WITHOUT the removal of a separated section is often done to improve the restorative prognosis of a tooth with gum disease between the roots or in the event there is a fracture between the roots of a multi-rooted tooth.
The hemisection and subsequent removal of a root from a multi-rooted tooth is called a ROOT AMPUTATION. The hemisection cut may be vertical, horizontal or diagonal. It is often used as a "bail out" procedure to salvage an existing crown or bridge
Since the cut to separate the tooth passes through the nerve chamber in the middle of the tooth, a root canal procedure must be performed prior to the split. If there is an existing root canal in the hemisected tooth, then all that is needed to seal the opening that communicates with the nerve chamber. This can done using a cap or a filling. The technique used will vary from case to case.
A RETROGRADE filling is a filling that is placed into the root end (apex) of a tooth. It is typically used when a traditional root canal procedure cannot be used or when a traditional root can procedure is not successful and the tooth cannot be treated in a convention manner again.
Hopefully, I've managed to answer your question as confusing as all this seems to be.
The photos left to right:
Retrograde filling, hemisected molar, hemisected molar under a bridge with one root amputated.
Regards,