Then why dive? Best way to not get bent is to not go under pressure.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Going tech - Patent Foramen Ovale (PFO) testing?
- Thread starter irsubmarine
- Start date
Please register or login
Welcome to ScubaBoard, the world's largest scuba diving community. Registration is not required to read the forums, but we encourage you to join. Joining has its benefits and enables you to participate in the discussions.
Benefits of registering include
- Ability to post and comment on topics and discussions.
- A Free photo gallery to share your dive photos with the world.
- You can make this box go away
No, The patient (tech diver candidate) is now informed they are in the high risk group for a DCI. They do NOT have to do anything.
They can ignore it all and carry on regardless.
Or they might decide NOT to waste a squillion dollars on tech equipment and training.
Or they might try to avoid DCI with special ascents and methods to lower the risk.
Or they could investigate further with more focused testing.
But the most important part, is we have likely prevented a future DCS injury, treatment and possible permanent injury. Is that not a good thing?
Oh and possibly we have also found a potential stroke victim later in life, too.
"An ounce of prevention is worth a pound of cure"
.
Go back and read my post here.
Ross, 7 days ago you sat in a room where a panel of experts, including the American cardiologist who probably closes more PFOs for divers than any other in the country, articulated exactly the same views as I am here. Think about that in the context of my comment above about cognitive dissonance.
Simon M
Go back and read my post here.
Ross, 7 days ago you sat in a room where a panel of experts, including the American cardiologist who probably closes more PFOs for divers than any other in the country, articulated exactly the same view views as I am here. Think about that in the context of my comment above about cognitive dissonance.
Simon M
I think your answer is confounding and confusing the issue. You are implying detection requires repair.... but that is not required.
No diver is under any obligation to fix the PFO's. Also there is no absolute right that we are able to scuba dive. Some people were not designed to be pressurized.
A PFO / shunt puts any diver at 5x higher risk for a DCI, than the rest of the population. New Tech divers should know about their personal risk factor, BEFORE they start on tech diving... not afterwards.
Someone said it cost $800 to do the TCD test? That's about the same price of a high end regulator. Not much room to complain about the price of TCD test, is there?.
.
You are implying detection requires repair.... but that is not required.
Of course not.
Go back and read my post here and try to understand it.
Then, if you want, continue to unintentionally advocate for the effective destruction of the technical diving industry.
If we as a medical community thought that the risk justified this, then we would advocate it too. But on the basis of the currently available evidence we don't .
I also think it is germane to remind readers that this whole "screen for PFO" campaign of yours has arisen out of the finding by multiple studies that bubble models (one of which you sell) result in formation of many venous bubbles (which are the harmful vectors that cross a PFO).
Simon M
Of course not.
Go back and read my post here and try to understand it.
Then, if you want, continue to unintentionally advocate for the effective destruction of the technical diving industry.
If we as a medical community thought that the risk justified this, then we would advocate it too. But on the basis of the currently available evidence we don't .
I also think it is germane to remind readers that this whole "screen for PFO" campaign of yours has arisen out of the finding by multiple studies that bubble models (one of which you sell) result in formation of many venous bubbles (which are the harmful vectors that cross a PFO).
Simon M
Ah yes... the blame everything on deeps stops / bubble models fallacy argument arises again......
NOTE: one cannot eliminate VGE, no matter how long one drags out the ascent, so your argument about bubble models is moot.
But a PFO does recirculate unfiltered blood, which contains excess N2 and He, that goes back into the tissue... so maybe there is more to this PFO-DCS problem than you imply.
And something that came up in the conference last weekend: two of your colleagues confirmed that arterialized VGE do NOT block at the tissue circulation (so your swiss cheese theory is not looking too good here - no peer support).
.
Last edited:
I chose to take the advise of Medical Professionals (here and during a dive physical) that work in the field and forego any PFO testing. Armchair experts and software developers are pretty far down on my list for medical advice. Now if had a question regarding C++, PHP or SQL, I would ask a developer.
NOTE: we cannot eliminate VGE, no matter how long one drags out the ascent, so your argument about VGE is moot.
We can certainly reduce them: a point clearly made by Neal Pollock in the expert panel session last weekend Ross.
But a PFO does recirculate unfiltered blood, which contains excess N2 and He, that goes back into the tissue... so maybe there is more to this PFO-DCS problem than you imply.
Another argument you have tried many times over the years, and every time I point you to the medical literature that demonstrates that the shunt fraction across a PFO is tiny (especially in during any degree of exercise) [1] and not materially important to exchange in inert gas. I also discussed this particular assertion of yours with Doug Ebersole last weekend and like me, he considered it a ridiculous explanation for the significance of PFO in the pathophysiology of DCS.
And something that came up in the conference last weekend: two of your colleagues confirmed that arterialized VGE do NOT block at the tissue circulation (so your swiss cheese theory is not looking too good here - no peer support).
I'm not sure what you mean by "block at the tissue circulation" but I will call you out on this one Ross. To my knowledge, no one has challenged the notion that venous bubbles crossing a PFO and entering the arterial end of tissue capillaries may cause harm, either by damaging capillary endothelium or by growing as supersaturated gas from the surrounding tissues diffuses into them (and therefore potentially arresting in the microcirculation rather than redistributing). These components of my "swiss cheese theory" have been published in multiple peer reviewed scientific journal articles (for example references 2 - 5).
So here is my challenge in response to your baseless claim: name those two colleagues and I will personally invite them here to explain their alleged comments, and we will see how accurately you are reporting their opinions.
Simon M
References;
1. Lovering AT, Stickland MK, Amann M, O’Brien MJ, Hokanson JS, Eldridge MW. Effect of a patent foramen ovale on pulmonary gas exchange efficiency at rest and during exercise. J Appl Physiol. 2011;110.2054-61.
2. Mitchell SJ, Doolette DJ. Pathophysiology of inner ear decompression sickness: potential role of the persistent foramen ovale. Diving Hyperbaric Med 2015;45:105-110.
3. Mitchell SJ, Doolette DJ. Selective vulnerability of the inner ear to decompression sickness in divers with right-to-left shunt: the role of tissue gas supersaturation. J Appl Physiol. 2009;106:298–301.
4. Ignatescu M, Bryson P, Klingmann C. Susceptibility of the inner ear structure to shunt-related decompression sickness. Aviat Space Environ Med. 2012;83:1145-51.
5. Wilmshurst PT, Byrne JC, Webb-Peploe MM. Relation between interatrial shunts and decompression sickness in divers. Lancet. 1989;334:1302-6.
Simon M
So here is my challenge in response to your baseless claim: name those two colleagues and I will personally invite them here to explain their alleged comments, and we will see how accurately you are reporting their opinions.
I'm not allowed to be argumentative any more... sorry. I have been blocked out of this thread once already. Can't risk it again.
You should resolve that conflict in professional opinions yourself - not my job.
Then, if you want, continue to unintentionally advocate for the effective destruction of the technical diving industry.
I think your profession would suffer more than mine. As you know, up to 50% of all DCS have some PFO or shunt involvement. Now imagine in a perfect world, these people did not dive, or where made to repair or to avoid conditions and the high risk and never got that injury in the first place?
You would have 50% less hyberbaric treatment patients. Of course more chambers would close too, so less demand for hyperbaric doctors.
The diving injury statistics would come down further, and divers could go back to following a proper formula derived deco schedule again, with confidence. No more need for the current puffed up schedules being promoted by some.
I don't see a down side to preemptive DCS prevention.
.
I'm not allowed to be argumentative any more... sorry. I have been blocked out of this thread once already. Can't risk it again.
You should resolve that conflict in professional opinions yourself - not my job.
What professional conflict? The one you have claimed exists but which you can provide no evidence for? I have provided you with multiple peer reviewed scientific journal article references that support a pathophysiological paradigm that you say has been verbally challenged but you refuse to identify the source of that challenge, and you are hiding behind the site TOS as a justification. How could politely substantiating your argument violate the TOS?
You have been backed into a corner of your own making and I put it to you that this sort of argument leaves you with no credibility left whatsoever.
I think your profession would suffer more than mine. As you know, up to 50% of all DCS have some PFO or shunt involvement. Now imagine in a perfect world, these people did not dive, or where made to repair or to avoid conditions and the high risk and never got that injury in the first place?
You would have 50% less hyberbaric (sic) treatment patients. Of course more chambers would close too, so less demand for hyperbaric doctors.
So, Ross, you think that mandating an expensive, invasive test, that has risks, which might cause problems for an individual's future career choices and insurance, that implies an increased risk of DCS for the individual whether or not that is actually true, and that is going to be positive in 25 - 30% of cases is going to do more harm to hyperbaric medicine than the technical diving industry?
It would do NO harm to hyperbaric medicine....
Do you know why it is increasingly hard to find a chamber to treat divers in the USA? It is because no one wants to treat them - not for financial reward anyway. It costs way more to provide an on-call diving medicine capability than you can recoup treating divers. That's why very few people are doing it. Less diving cases will do no harm whatsoever to hyperbaric medicine, whose practitioners spend 99% of their time treating non-healing problem wounds and radiation tissue injury.
The diving injury statistics would come down further, and divers could go back to following a proper formula derived deco schedule again, with confidence. No more need for the current puffed up schedules being promoted by some.
That's one of your problems Ross. Immutable belief in formulae that were derived with very limited testing decades ago when no-one was doing two decompression dives a day for 10 consecutive days.
Simon M
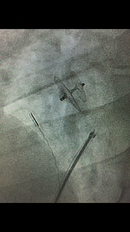
DCS II twice with the 2nd time being much worse. Both events had dive times approaching 3 hours with long periods of 90’-115’. The first time was after Bozel Spring and showed itself about 2 hours after surface. The 2nd time was at another spring on the Chipola River and came on about an hour after surface. Luckily I was able to be ground transported quickly both times and flown to Mobile, AL the 2nd. Tested negative TTE and positive with TEE. Dr. Ebersole closed it 12/27/16 and I haven’t had any problems since but haven’t been able to dive as much since taking a new job January 2017. DCS risk is considered lower but can still happen on any given day. As previously said, having the PFO closed doesn’t make anyone DCS proof. I haven’t noticed any difference in post diving fatigue however I used to get migraines w/ aura every couple months and haven’t had one since having it closed. The picture is the PFO Occluder implant. Not a great picture but someone in the OR took a picture with a cell phone.
Attachments
Last edited:
Similar threads
- Replies
- 4
- Views
- 528
- Replies
- 11
- Views
- 1,538
- Replies
- 3
- Views
- 676